Attention Deficit Hyperactivity Disorder (ADHD) remains a prevalent neurodevelopmental disorder among children in the United States, often extending into adulthood. Drawing on data from the CDC – Centers for Disease Control and Prevention, this article delves into the evolution of ADHD diagnosis rates and treatment modalities, revealing the nuanced understanding and approach towards this disorder across different American states.
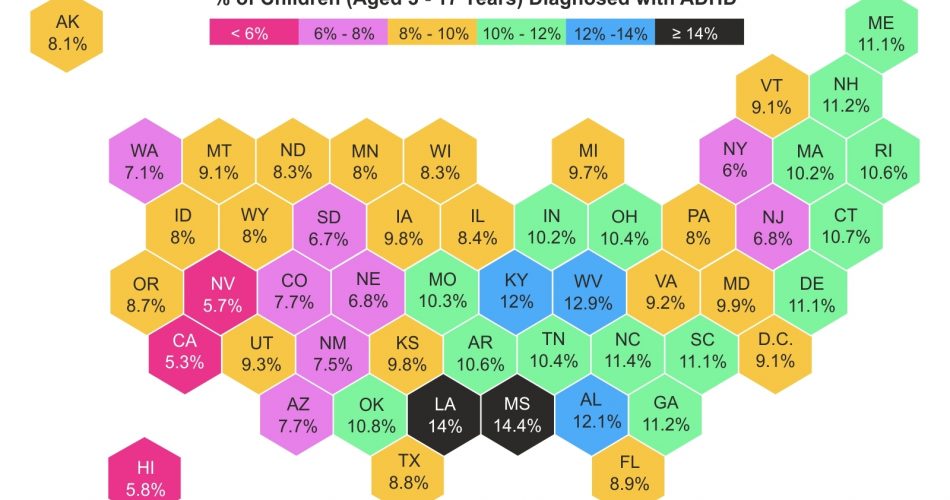
Current Diagnosis Rates
Recent statistics from 2016 to 2019 provide insights into ADHD’s prevalence across different American states. While the national average diagnosis rate teeters around 10%, there are noteworthy variances among states. Louisiana and Mississippi stand out with elevated rates of 14% and 14.4% respectively, hinting at a higher occurrence or perhaps heightened diagnostic practices. In contrast, states like California (5.3%), Nevada (5.7%), and Hawaii (5.8%) report lower rates, possibly suggesting differential accessibility to healthcare or varying levels of public awareness about ADHD.
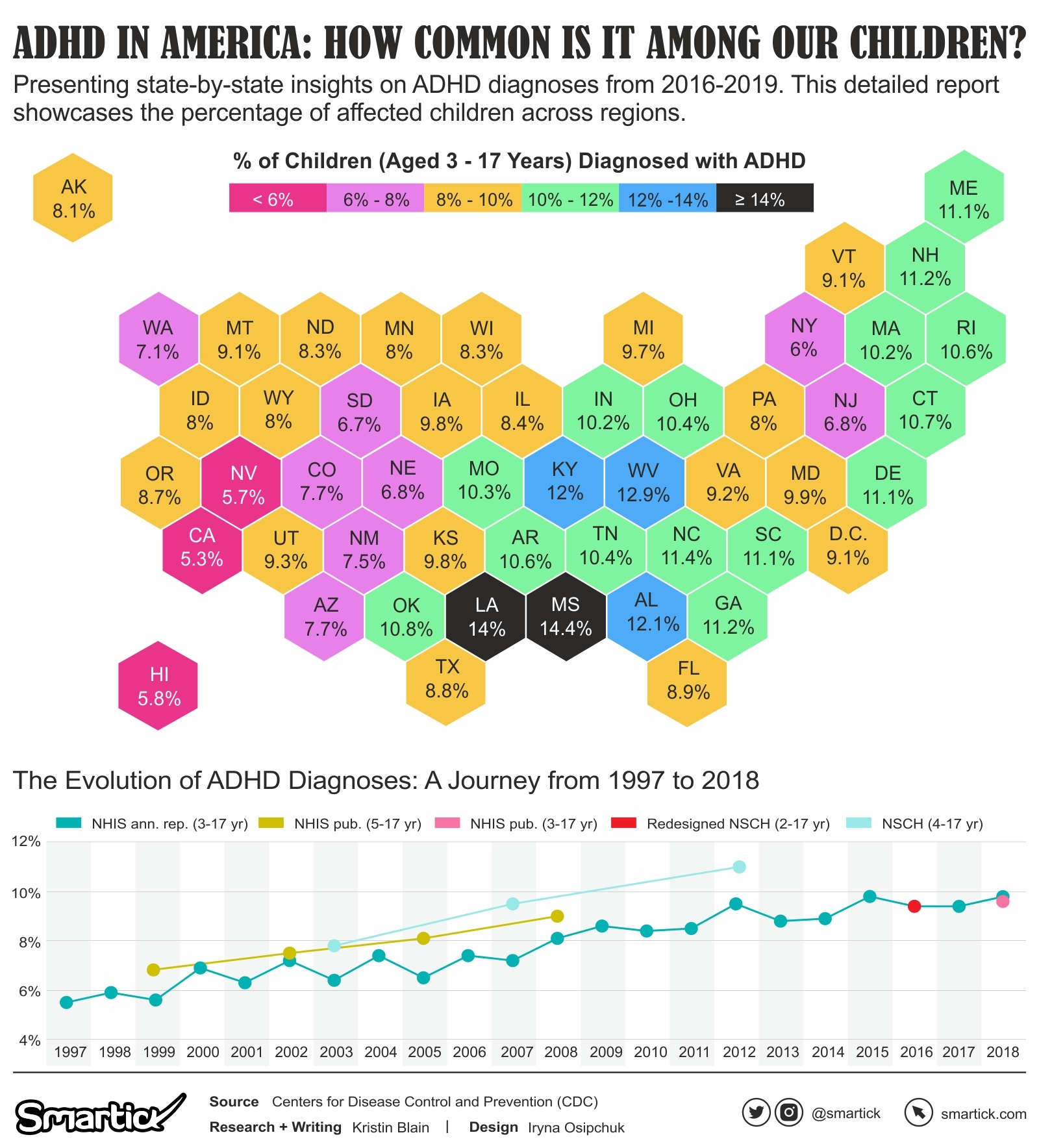
Historical Diagnosis Rates (1997-2018)
From 1997 to 2018, the diagnosis rates among U.S. children aged 3-17 years experienced a consistent rise. The rate that stood at 5.5% in 1997 increased to 9.8% by 2018, with significant surges observed in 2000, 2008, and 2012. These increases potentially underscore changes in diagnostic criteria, increased healthcare accessibility, or broader societal recognition and understanding of ADHD.
A Spectrum of ADHD Treatments
As our understanding of ADHD has deepened over the years, so have the approaches to its treatment. Treatments encompass a spectrum, ranging from pharmacological interventions to behavioral therapies. Medication, particularly stimulant-based, remains a cornerstone, enhancing focus and reducing impulsive behavior. Meanwhile, behavioral therapy aims to equip children with coping mechanisms, structure their behavior, and improve their social interactions. For many, a combination of medication and behavioral interventions produces the best outcomes. Moreover, there’s a growing emphasis on comprehensive mental health treatments, ensuring a holistic approach to managing not just ADHD, but also the associated emotional and behavioral challenges. With this backdrop, let’s dive into the data to understand how children with ADHD are being treated across the U.S.
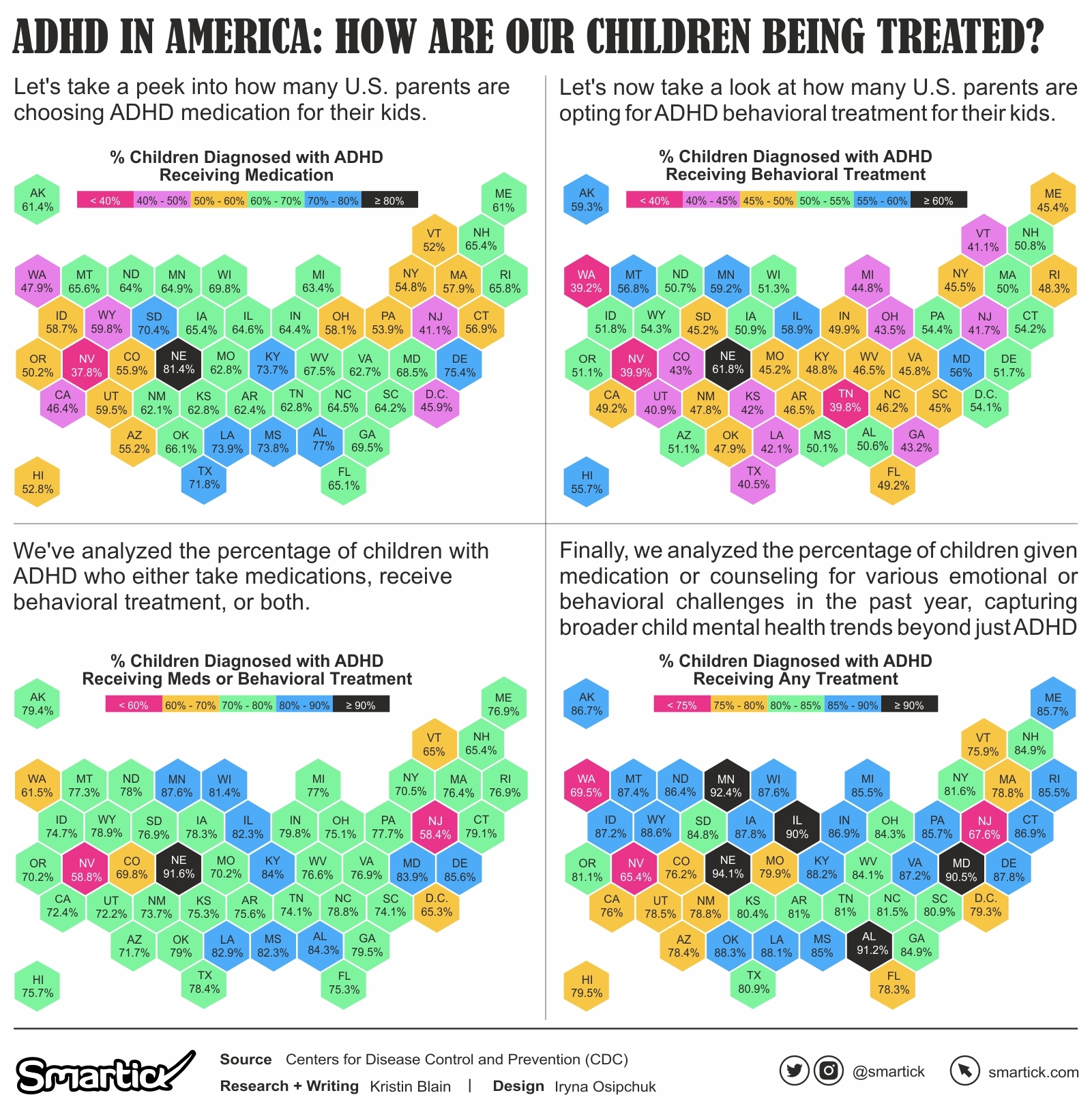
ADHD Medication Treatment
Medical intervention is a prevalent route taken to manage ADHD. Between 2016 and 2019, the distribution of ADHD medication treatment varied significantly across states. Nebraska (81.4%), Alabama (77%), and Delaware (75.4%) exhibited the highest percentages, suggesting a possible preference for medication-based treatments or an increased prevalence of severe ADHD cases. Meanwhile, states like Nevada (37.8%), New Jersey (41.1%), and California (46.4%) reported lower percentages, potentially pointing towards alternative treatment preferences, skepticism about medication, or different healthcare guidance.
ADHD Behavioral Treatment
Behavioral therapy remains a cornerstone treatment for ADHD, focusing on aiding children in developing coping mechanisms and structuring their behavior. The 2016-2019 data depicts:
- Nebraska leading with 61.8%, followed closely by Minnesota (59.2%) and Alaska (59.3%). Such high rates might be indicative of a robust healthcare infrastructure supporting therapy or a cultural inclination towards non-medical treatments.
- On the flip side, Nevada (39.9%), Washington (39.2%), and Utah (40.9%) report lesser percentages, potentially due to limited access to behavioral therapists or varied health insurance coverage.
Comprehensive Mental Health Treatment
The overall mental health landscape for children with ADHD and other conditions is crucial. The data reveals:
- An overwhelming majority of states saw over 75% of children receiving some form of mental health treatment. Notably, Nebraska was at the forefront with 94.1%, emphasizing the state’s comprehensive approach to child mental health.
- Conversely, states like Nevada (65.4%) and New Jersey (67.6%) recorded lower rates, highlighting possible gaps in mental health awareness or service accessibility.
The multifaceted ADHD data offers insights into the progression of its diagnosis and treatment across the U.S. over the years. The discrepancies in treatment choices across states suggest a lack of a universal approach, influenced by an array of factors, from healthcare infrastructure to cultural perspectives. While we’ve made significant strides in understanding and treating ADHD, there remains an ongoing need to bridge treatment gaps and ensure holistic, consistent care for every child, regardless of their geographic location.